Living with Chronic Pain and an Eating Disorder
July 21, 2025 | By Carissa Hannum
This is a repost of our blog originally posted in 2023.
The Battle of Living with Chronic Pain and an Eating Disorder
The last week of February is National Eating Disorders Awareness Week, March is Disability Awareness Month, and September is Pain Awareness Month. These observances spotlight important public health issues and for many individuals, chronic pain and eating disorders are deeply interconnected.
Living with a disability takes work and navigating support options can be exhausting. A subset of disability includes living with invisible illnesses like chronic pain, which can be physically and mentally draining. Finding ways to cope with chronic pain can be isolating and lead to feelings of helplessness. While not always talked about, chronic pain can also trigger or worsen eating disorder symptoms, as individuals may seek control or relief through disordered eating.
Unfortunately, as an eating disorder progresses, it can intensify chronic pain symptoms or even lead to the development of a chronic illness that didn’t exist before. This blog explores the connection between eating disorders and chronic pain and to help raise awareness about their overlap.
What Is Considered Chronic Pain?
The Mayo Clinic defines chronic pain as: “Chronic pain is pain that lasts for over three months. You may feel the pain all the time or it may come and go. It can happen anywhere in your body and has countless causes.”
The pain is a somatic experience, felt physically in the body. Many people often describe their pain using descriptors like stabbing, burning, shooting, sharp, pulsing, or stinging. While sudden pain can be a warning that something is “wrong” in the body, chronic pain often stems from disease or progressive illness or injury and can be constant or come and go.
Examples of chronic pain include (but are not limited to):
Migraines and headaches
Nerve pain, such as neuralgias and neuropathies, such as fibromyalgia
Cancer pain
Arthritis and other joint or muscular pain
Back pain
Stomach and Gastrointestinal issues, such as inflammatory bowel syndrome (IBS)
Pain affecting women such as endometriosis, vaginal pain other pain related to the menstrual cycle
Chronic fatigue syndrome
Bladder pain, such as cystitis
And many more! If your pain isn’t listed here does not make your pain experience any less real or valid.
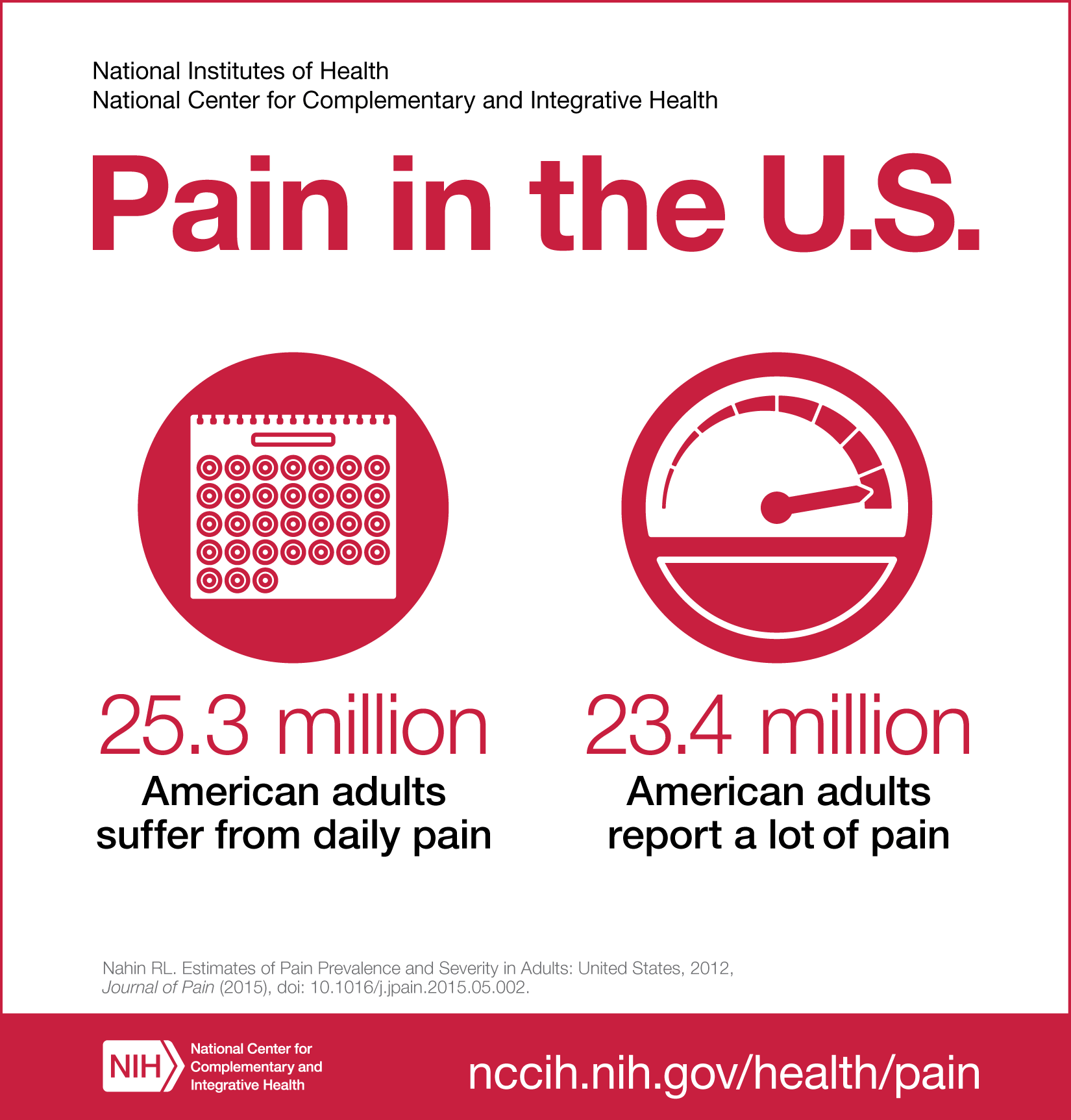
The Severity of Chronic Pain
Chronic pain is a public health crisis. According to a 2012 study, the National Institutes of Health found that ~25.3 million adults experience chronic pain which means that they had pain every day for the preceding 3 months, and 23.4 million report feeling “a lot of pain” every day.
Another study that was conducted by the Centers for Disease Control and Prevention in 2019-2021 estimated 20.9% of U.S. adults (51.6 million people) experienced chronic pain, and 6.9% (17.1 million people) experienced high-impact chronic pain, defined as pain that substantially limits daily activities. The study also found higher prevalence rates among non-Hispanic American Indian or Alaska Native adults, adults identifying as bisexual, and those who were divorced or separated.
The U.S. Pain Foundation has done extensive research within the medical community. The foundation estimates that 1 in 4 Americans experience pain every day and notes that there are not enough board-certified pain specialists available to meet the growing demand for treatment. It estimated that there is currently only 1 specialist per 10,000 chronic pain patients.
Unfortunately, the struggles of those suffering from chronic pain are often overlooked. In addition, funding for chronic pain research is severely lacking, and existing treatments typically provide only about 30% relief for most patients.
With the gaps and lack of support with chronic pain treatments and medical professionals, many individuals living with chronic pain can feel as though they are dealing not only with physical pain but also emotional pain. The combination of physical and emotional pain can leave a person feeling hopeless, helpless, out of control, and frustrated with their options. Many of my own clients have turned to or developed an eating disorder as their own form of coping and way to feel in control of their health.
The Mind-Body Connection: Coping Through Eating Disorders
The mind and body are closely connected and correlated. Due to the mind and the body having a reciprocal relationship, daily functioning and mental health can be affected significantly due to pain. The more pain that an individual experiences, the more likely an individual can experience significant mental health decline and emotional dysfunction.
Individuals’ that suffer from high levels of pain suffer often report:
Suicidal ideation
Sleep disturbances
Social and family dysfunction
Loss of independence
Isolation and discrimination
When emotions feel overwhelming or dismissed by providers, an eating disorder can become a coping mechanism. Whether it's anorexia, bulimia, binge eating, or another disordered behavior, the eating disorder may serve as a way to distract from or control the pain. Because pain is a somatic (bodily) experience, people with chronic pain may become disconnected from their bodies—especially when the body feels unsafe or out of control. Some clients express that when medical treatments aren’t effective, they feel their only option is to take matters into their own hands. For some, that means using food or restriction as a way to disconnect from the pain.
Eating itself can become traumatic, particularly when pain is triggered by food. In these cases, nutritional support is a critical part of healing from both chronic pain and an eating disorder.
These emotions, when left untreated, can feel out of control and chaotic. An eating disorder can become an ideal coping mechanism especially when their pain is overlooked or not helped by certain medical treatments and/or professionals. The eating disorder, whether that be anorexia nervosa, bulimia nervosa, binge eating disorder, or any form or combination of eating disorder symptoms, can be a distraction from pain and means to control the immense pain a person is experiencing.
As stated earlier, chronic pain is a somatic experience in the body. Although understanding physical sensations in the body can be a helpful experience to identify issues or emotional needs, physical sensations can become confusing for someone experiencing chronic pain. For instance, a sharp shooting pain for someone that doesn’t experience pain daily can signal the need for rest or the need to go to the doctor. For someone with chronic pain, feeling as though there is always danger can lead a person to feel as though their body is an enemy.
Many people think, “If I’m not feeling helped by the medical treatments being recommended to me, I might as well take my health into my own hands”. Many people describe that the only way to control their pain is through disconnecting from their body through use of an eating disorder. In addition, for those that suffer pain due to eating, a basic need such as fueling the body can be a traumatizing experience. Finding support to meet nutritional needs in all these situations is very important to recover from chronic pain and an eating disorder.
The Impact of Medical Misinformation and Shame
Unfortunately, many healthcare providers are not trained to recognize the overlap between chronic illness and eating disorders. As a result, stereotypical or uninformed medical care can unintentionally contribute to the development or worsening of disordered eating.
For instance, some people are told to lose weight, try restrictive diets, or are given oversimplified advice. This can not only invalidate the severity of an individual's pain, but could cause a person more emotional distress for feeling as though they are to “blame” for their pain.
Shame can be a highly distressing emotional experience that leaves many people feeling as if they were responsible for their pain. Again, the eating disorder becomes an emotional outlet to numb from both the physical pain and the emotional shame.
One of the most difficult concerns for someone with chronic pain is having to adjust to having different needs from the “normal” population. The sheer act of approaching a medical provider for help with chronic pain is already difficult. When those efforts are dismissed and cannot be helped, many people will internalize the idea that their needs are “too much.” In these moments, an eating disorder may seem like the only way to make those needs disappear. But over time, those unmet needs only build up, causing deeper pain and emotional distress. Those with chronic pain need to learn to identify and find ways to meet both the physical needs of chronic pain and their emotions.
Can Eating Disorders Cause or Worsen Chronic Pain?
While eating disorders may offer short-term relief and comfort for individuals experiencing chronic pain, eating disorders often contribute to long-term health issues. Some individuals may have never experienced chronic pain until the development of their eating disorder. Though eating disorders are mental health conditions, they can lead to physical complications when left untreated. When left untreated, an eating disorder can cause chronic pain issues such as:
Gastrointestinal issues
Joint pain
Headaches
Fatigue
In addition, because an eating disorder is not helping clients learn appropriate methods of dealing with their pain, an eating disorder and chronic pain can be an endless vicious cycle. Pain fuels disordered eating, which increases pain and emotional distress. The short-term gains can lead to long term issues in daily functioning such as:
Worsening depression and anxiety
Negative self-beliefs
Difficulty managing daily life
Increased isolation and shame
What may feel like a helpful disconnection in the beginning of an eating disorder often results in deeper suffering over time with long term chronic pain complications and increased mood concerns like depression, anxiety, shame, as well as difficulty accepting help for needs.
The Need for Treatment and the Importance of Mindful Embodiment
Since eating disorders often stem from a desire to control and disconnection from painful experiences, mindful and embodied methods of approaching both the eating disorder and chronic pain is imperative. Learning how to accept the emotions related to chronic pain and one’s eating disorder can help ease physical pain over time. The goal of psychotherapy for chronic pain is to help clients not only gain support and relief from their pain but also to accept the pain as part of life to ease psychological and emotional effects. Becoming more embodied is being more aware of and connected to the body, which is not always comfortable. But with the right therapeutic intervention, it is possible.
One form of therapeutic intervention that can be helpful for mitigating the effects of chronic pain is Acceptance and Commitment Therapy (ACT). ACT helps distinguish not only acceptance of the illness and chronic pain, but helps individuals distinguish between “clean pain” and “dirty pain”
Clean pain refers to the natural, unavoidable discomfort that comes with being human such as grief after a loss or disappointment after a failure.
Dirty pain arises when we try to resist or avoid clean pain such as, “I’m lazy due to my pain” or “I’m not good enough due to my pain.” This avoidance can lead to secondary suffering, like guilt, shame, or prolonged sadness.
In therapy, the focus is on helping clients learn to accept clean pain as a part of the human experience, rather than fighting it, which in turn can reduce the intensity of dirty pain over time.
Supportive Strategies for Healing from Chronic Pain and Eating Disorders
Learning to become more embodied and mindful can be a scary process. For those living with chronic pain, being in a body that has felt harmful or unsafe can be terrifying. Separating and identifying emotional pain from physical pain is often an important first step in the healing journey. Rebuilding a relationship with the body can feel overwhelming or even chaotic at times which is why it is necessary to have a team of professionals that can help treat both the chronic pain and the eating disorder.
Some treatment approaches may include:
Creating a plan for value-oriented activities, those that align with a client’s personal values and bring meaning to their life. Clients may need to “dose” or pace these activities to prevent pain flare-ups, but avoiding them entirely can increase emotional suffering and, in turn, physical pain.
Practicing self-compassion, especially during moments when eating disorder symptoms arise. Offering kindness instead of judgment helps reduce shame and supports long-term healing.
Identifying and naming emotions in situations where eating disorder behaviors would have previously been used as coping tools.
Building flexibility around beliefs tied to “dirty pain” and reframing self-critical thoughts and cultivating positive self-talk to reduce emotional suffering.
Developing mindfulness techniques to use during pain flare-ups can help clients stay grounded and reduce reactive behaviors.
Recognizing triggers for chronic pain episodes and learning alternative ways to respond, rather than turning to disordered eating for relief.
Finding ways to soothe the body, rather than criticize or disconnect from it, during difficult moments, such as using warmth, gentle movement, or comforting sensory tools.
Allowing the use of daily comfort strategies, such as a supportive back pillow, mobility aids, or routines that reduce physical strain and increase day-to-day ease.
Exploring new meaning and identity as someone who lives with chronic pain. This may include processing grief and loss around how pain has changed one's life.
Celebrating the body for what it can still do, even when it feels like pain has taken so much away. Small victories and acts of care matter.
Expressing the emotional weight of chronic pain, including anger, sadness, loneliness, or frustration in healthy and validating ways.
Learning to label both emotional and physical sensations. In therapy, being able to name what is happening in the body can help reduce overwhelm. This is especially important, as eating disorders often create a sense of dissociation from the body and its needs.
Considering psychotropic medication when appropriate, to help manage symptoms of depression, anxiety, or other mental health conditions that may accompany chronic pain or disordered eating.
You Deserve Help and Healing
If you're living with both chronic pain and an eating disorder, you are not alone and you are not too much. Please reach out to a therapist, doctor, or any other professional who understands the complex relationship between chronic pain and eating disorders and inquire about treatment. It is a very brave thing to discuss both your eating disorder and your chronic pain. Whether your pain was a problem prior to your eating disorder or increased due to an eating disorder, it is essential to find a team of professionals who can help you understand the intricacies around how your chronic pain and eating disorder impact one another and your recovery process. Help is available. Recovery is possible.
Reach Out
If you’re considering professional support, we’re here to help. Please reach out to schedule a free, no-commitment consultation. There’s no fee and no obligation—just click the button below to get started.
You can also call or text us at 202-656-3681, or email us directly. Give yourself the opportunity for the support you deserve.